Our Health California
To better meet Our Health California’s goals of working toward an equitable, accessible health care system across our state, we’ve folded our website into that of our parent organization, the California Hospital Association. We’re focusing less on general health tips and more on patient stories and hospital innovation across California, as well as actions you can take to improve the health care system. Check out our hospital stories below!
The Latest
All Stories
-

Patients See “Superior Outcomes” from Blood & Marrow Transplants
Hospitals in Action -

A-Fib Patients Receive Game-Changing Treatment
Hospitals in Action -

Surgical Excellence Saves a Father’s Life
Hospitals in Action -

Stem Cells Offer Veterans a New Lease on Life
Hospitals in Action -

Determined Septuagenarian Bodybuilder Gets a New Spine
Hospitals in Action -

Gene Therapy Sets Baby on a Remarkable Path to a Normal Childhood
Hospitals in Action -

A Long Journey to Family Practice
Hospitals in Action -

Experimental Procedure Aims to Eliminate Seizures
Hospitals in Action -
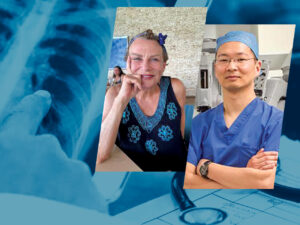
Fortunate Timing Aids Lung Cancer Treatment
Hospitals in Action -

Bonding with Newborns Meets International Kangaroo Awareness Week
Hospitals in Action -

COVID-19 Archive Chronicles Pandemic Memories
Hospitals in Action -

Heart Patient Returns to Making Movies
Hospitals in Action